Plasmatherapies
The term plasmapheresis encompasses different techniques (filtration or adsorption on plasma), which remove only specific elements contained in the plasma, allowing treatment of a large number of diseases.
TPE
Therapeutic Plasma Exchange
in case of
Auto-immune diseases
Rejection of transplanted organs
Intoxication
TPE is usually performed with 5-10 consecutive sessions of 1-2 hours.
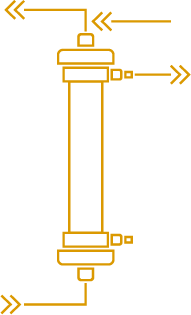
TPE involves the removal of the patient’s plasma from the blood and the replacement with fluids which do not contain the large substances, such as antibodies, targeted for removal. It applies to a wide range of acute diseases and also to chronic ones although more rarely due to the adverse effects of the replacement fluids, human albumin or fresh frozen plasma, overtime.
Technically speaking
HP
Hemoperfusion
in case of
Ulcerative colitis
Crohn disease
Inflammatory Mediator Removal
Hemoperfusion can be used for both acute and chronic diseases, such as cascade filtration, and with the same frequency; 5 to 10 consecutive sessions of 1-2 hours.
Hemoperfusion can be used to directly remove specific substances from the blood by adsorption, a technique which fixes substances on a surface. It is of particular interest for leukocytes which are too big to be filtrated without major loss of red cells.
Technically speaking
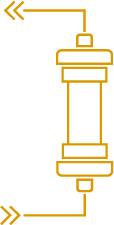
In hemoperfusion, blood is passed through a sorbent that retains the substances for which it is specifically designed. At the end of the treatment, the sorbent contains large amounts of this substance and is discarded. The sorbent directly interacts with the blood which is more prone to lead to some clinical side effects, such as bradykinine release, than plasma. Side effects and potential contraindications shall be pointed out by the manufacturer of such sorbent.
A bit of
HISTORY
Plasmatherapeutic procedures were performed for the first time at the beginning of the 20th century and become more readily applied during the 70’s all over the world.
The first plasmapheresis was performed in Russia in 1913 by Yurevitch and Rosenberg to demonstrate the concept of “ … washing the blood outside the body …”. It consisted of extracting a portion of a rabbit's blood which was then centrifuged to separate the red blood cells. These were then mixed with normal saline which was heated before being reinjected to the rabbits.
However the term plasmapheresis was defined by Pr John Abel in USA in 1914, combining two terms :
- Plasma: liquid part of the blood
- Aphaeresis: In Greek “removal
Thus, plasmapheresis was defined as a method of removal of plasma from an organism.
Unfortunately, the First World War began which stopped the experimentation and this technical approach was forgotten for a few decades.
In 1944, the Swedish physician Jan G. Waldenström described a case of Macroglobulinemia with symptoms of increased blood viscosity. In 1955, he performed effective plasmapheresis procedures on a patient with macroglobulinemia and noted an effective reduction of macroglobulin in the blood.
In 1963, several procedures were successfully performed on patients with Waldenström illness (Macroglobulinemia with high blood viscosity) which can be considered as the first regular application of plasmapheresis to a human disease.
Plasmapheresis is regularly performed in many countries since the 70’s with approximately 1000 procedures in England, 6200 in France and later in the 80’s with 50 000 procedures per year in the USA.
Today the term plasmapheresis encompasses different techniques (filtration or adsorption on plasma), which remove only specific elements contained in the plasma, allowing treatment of a large number of diseases.
Some therapies or options are approved for certain territories only.
Please contact us for more information.
Hot topics

ERA 2026
Join us to the 63th European Renal Association (ERA) Congress in Glasgow, Scotland. ERA is based on 3 pillars: Education, Science and Networking. As Infomed, we support the association for more than 20 years and we clearly appreciate to be a key partner to the association to develop excellence and quality of the scientific knowledge.

EDUCATIONAL VIDEOS
Discover Infomed’s educational videos with presentation from basics of blood purification to internationally renowned professor physician’s interview and discover all the interest of various application of therapeutic technics offered by Infomed’s solutions.
Kidney Week Denver
Come and share with us the Kidney Week organized by the American Society of Nephrology (ASN), in November in Denver, Colorado. This key event is focus on education, training and knowledge sharing, through a large number of publications. Once again, we are pleased to support and take part by supporting the exchange of the international know-how in the field.